News at Telecare
Links We Love: National Recovery Month
/Each year, Telecare joins SAMHSA (Substance Abuse and Mental Health Services Administration) in celebrating National Recovery Month. The 2017 Recovery Month theme, “Join the Voices for Recovery: Strengthen Families and Communities,” highlights the value of peer support by educating, mentoring, and helping others. People in recovery are encouraged to share their personal journeys and connect with others on SAMHSA’s forum.
- Download and share the infographics we created: Suicide Prevention: Facts and Risks and Suicide Prevention: Facts and Risks for Youth
- Check out SAMHSA’s event calendar to find out what’s happening in your area for National Recovery Month.
- Download SAMHSA’s Recovery Month Toolkit or EachMindMatters Suicide Prevention Activity Tip Sheet for ideas on reaching out to your community and spread awareness around these issues.
OC AOT Open House
/On June 1, the Orange County Assisted Outpatient Treatment (AOT) program in Santa Ana, California, welcomed the community to celebrate at their open house hosted in their new facility.










Guests included the AOT judge, county counsel, public defender's office, members and their loved ones, a representative from First District Supervisor Andrew Do's office, and other Telecare program staff.
The open house featured a fun photo booth and a slideshow with information about the program's success, staff, and highlighted a few of the program participants. "The open house had a great turnout," said Administrator Anna Bowes. "We look forward to continue servicing the communities in Orange County!"
Telecare's Orange County AOT program opened in November 2014 and expanded in July 2016. This community-based program is based on the Assertive Community Treatment (ACT) model and prescribed for adults with serious mental illness who are experiencing repeated hospitalizations or incarcerations, but are not engaging in treatment. AOT services include intensive case management, housing assistance, vocational and educational services, medication support and education, co-occurring services, and 24/7 support and availability.
Administrator Career Opportunities
/Telecare's leadership team is growing in Kern and San Bernardino counties in California!
We are looking for administrators for the following programs:
- East Kern County Crisis Stabilization Unit (CSU) Administrator
- San Bernardino Crisis Residential Treatment Administrator
- San Bernardino West Valley CSU Administrator-RN
- San Bernardino CSU East, Administrator-RN
Telecare's program administrators have the opportunity to guide their teams in delivering outstanding service, while continually improving the program with new and innovative clinical, operational, and technology-based approaches to streamline care, treat the whole person more effectively, and empower staff with greater skills, tools, and resources to support powerful change in consumers’ lives.
Links We Love: Mental Health & School
/- The first day of school is just around the corner for many college students, and with one in five students living with a mental health condition, it is important to know who to contact for help & resources.
- Click here for Center for Online Education's mental health resource list, as well as links to health and social services departments for each state
- NAMI has created an online forum for young adults to talk about their experiences and de-stigmatize mental health
- Each Mind Matters has created a resource page for young adults either in college or transitioning out of college
New Exhibit Showcases Artists with Mental Health Diagnoses
/On August 18, artists from around Sonoma County came together to showcase their artwork for the opening night reception of the exhibit Out of the Shadows: A Collection of Transformative Art. The exhibit highlights the artistic contributions of mental health consumers from around the area, including four members of Telecare’s Sonoma ACT program.
Sonoma act artists (from left to right) Arlo y., ben, and phil mcclary. For the out of the shadows exhibit, Arlo contributed a drawing, ben contributed a poem, and phil contributed a watercolor painting.
Out of the Shadows was put together by the Sonoma County Wellness Art Collaborative, a collective of mental health service providers who offer vital support to individuals in their community. Witnessing the brilliant works of art depicting the transformative process of a person’s journey toward recovery, the wellness collective wanted to showcase their member’s talents and bring the work “out of the shadows” to recognize the creative contributions of our community.
The event was recently covered in a local newsweekly, the Bohemian.
"Culturally, we appreciate our artists who have eccentricities, but I don't know that we really appreciate our eccentrics who have artistic abilities," said Adam Kahn, a founding member of the wellness art collective, while talking to the Bohemian. "And a lot of the folks we work with do have those artistic abilities. Their way of being in the word is so unique, but oftentimes it's not something that's appreciated by the mainstream. A lot of that expression is shoved into corners or dark places."
On opening night, more than 200 members of the community turned up to see the exhibit, alongside live performances of poetry, song, puppetry, and comedy. This is the first event from the Sonoma County Wellness Art Collective, and with the great turn out, interest, and community building, the collective plans on more events in the future.
Admission to Out of the Shadows is free to the public, and 100% of the proceeds from the sale of the artwork will go to the artists. The exhibit will be on display at the Steele Lane Community Center in Santa Rosa, California, from August 18 through October 15, 2017. For more information, visit the Sonoma County Wellness Art Collaborative Facebook page by clicking here.
August Leadership Announcements
/We are thrilled to welcome and congratulate our new administrators and promoted staff!
New Hires & Promotions: May
/We are pleased to welcome and congratulate the following Telecare employees:
The Power of Hope: How Peer Services Provide Living Examples of Recovery
/Erin "Wesa" Arthur is a PSC III Substance Abuse Specialist at Telecare’s Santa Maria ACT program.
Wesa specializes in addiction and co-occurring conditions among members and helps them through psychoeducation, assists in detox treatment, and conducts general case management. She uses harm reduction, the RCCS, and shares her story to instill hope.
"That is why I am so passionate about recovery and the work that I do—I’ve been there," said Wesa. "I have 28 years of sobriety and I am living with a mental illness and co-occurring disorders. I think that it helps clients when I open up with them about my own experiences."
Having the ability to have the challenging conversation surrounding substance use in a non-judgmental fashion is key for building trust and hope among our clients. "I think there is so much doubt that many people who are struggling with co-occurring disorders face and that it is something that is destined to hinder them, and that’s not true," Wesa said. "Like anything in recovery, it’s a process and it’s unique to every individual."
This year, Telecare has been expanding and improving the way we inform our staff about co-occurring disorders. With our online learning portal, we are now able to offer staff training sessions on substance use that they can access at any time to help with their understanding of dual diagnosis among clients and how to start conversations around these topics. More than 70% of Telecare programs successfully completed COEG facilitator training and launched COEG groups for the people they serve.
Wesa had the opportunity to share her own experiences when COEG was first being developed. "I feel so strongly that until someone is clean and sober, it’s extremely difficult to treat the psychiatric disorder,” she said. "Substance use can have such an impact on mental health symptoms. To provide adequate treatment for people who have a co-occurring disorder, you have to take the time to understand how the two are affected by one another."
Today, Wesa continues her interest in psychology and writes about her experience. Her recovery journey is a reminder to those she works with that anything is possible.
"People gave up on me when I was diagnosed with bipolar disorder, and I proved them wrong," she said. "The thing I love is being able to instill hope and show them by example that anything is possible. And I love the clients. I absolutely love the clients we serve."
SUTS Telemedicine Detox Pilot
/Recovering from addiction can be an extremely stigmatizing and isolating experience for many of our clients. Telecare recently conducted a pilot on Telemedicine Detoxification (Tele-Detox) to see if we could help clients overcome this isolation, while getting the right treatment support at their own pace, in the safety of their own home or within a program.
“Tele-Detox is detox treatment provided via live video calls at the convenience of where our clients are,” said Scott Madover, Director for Specialty Product Services, Substance Use Treatment Services (SUTS). “Through this online process, clients can get connected with an addiction physician who can walk them through their detox, answer any of their questions, and prescribe medications so that their substance use withdrawal symptoms can be as mild as possible.”
The nine-month pilot started June 2016 and was conducted at our CHANGES program in Oakland, CA. CHANGES is Telecare’s first co-occurring program and has been instrumental in helping Telecare identify effective and collaborative ways to treat co-occurring substance use disorders. CHANGES clients receive both mental health and substance use services, but in this program, are not required to be abstinent. Staff encourage clients to reduce their substance intake through a harm reduction model and can refer clients to more robust inpatient detox services.
The Tele-Detox program came about because we wanted to help clients overcome the isolation of addiction recovery, while getting the right treatment support at their own pace, in the safety of their own home or within a program.
The Tele-Detox approach is promising because it supports these goals, as well as offers other system benefits. It’s less expensive than inpatient detox, enables clients to start the detox process faster because it does not require waiting for an available inpatient bed, and alleviates pressures on those inpatient beds for people who need inpatient care the most.
Through the Tele-Detox process, clients are screened and connected with an addiction physician through Clinics On Demand. Clients are loaned a personal computer or a tablet if they do not already have one, a blood pressure cuff, and a finger oxygen device. The blood pressure and finger oxygen devices connect automatically and wirelessly with a monitoring system at Clinics On Demand.
Clients who participated in the demo had regularly scheduled telephone visits with physicians and clinical staff to discuss progress, address concerns, resolve problems, and refer to higher level of care if needed. CHANGES staff could contact the client’s physician to report any change of condition they observe during the detox treatment. Once detox treatment was completed, CHANGES staff would help and support clients in their chosen Intensive Outpatient Programming (IOP) treatment in addition to the services at CHANGES.
“Although the turnout for the pilot program was modest, the support and encouragement clients received by participating really helped them understand their addiction,” Scott said. “As a company, we are looking to continue to have the opportunity to build expertise within Telecare around substance use for our staff.”
Michelle Norris worked on the Tele-Detox program pilot when she was a Personal Service Coordinator II at CHANGES. As someone with lived experience herself, she knows that there is a lot of stigma surrounding addiction, and that having more personalized access to help can make taking those first steps towards recovery a little easier.
“There's still a lot of misconceptions around addiction, like the thought that people could just stop if they wanted to,” she said. “You know what? If I could've stopped, I would have, but I couldn't until I got more education. Having the right education and being provided the steps you need to take to help the client is so important because recovery can be a lot harder than you think.”
Michelle uses the experience from her own recovery to help guide others on their journey. She is now a Licensed Clinical Social Worker (LSCW) at Telecare’s Villa Fairmont Mental Health Rehabilitation Center.
SUTS: Expanding Treatment at Telecare
/Our Plan for Building Skills, Staff, Practices & Programming
In January 2017, Telecare finalized a three-year plan to enrich and expand our substance use treatment services (SUTS) capabilities, with a specific focus on people who have a serious mental illness (SMI) and co-occurring substance use issues.
"Traditional substance use agencies are not necessarily prepared to serve people who have SMI," said Faith Richie, SVP of Development. "We have a 50-year history of working with SMI and complex needs and in the last few years, have made major steps forward in our ability to recruit, retain and support licensed staff, particularly psychiatrists, through our TLC Physician Services Organization. This will make it easier for us to step into more direct SUDS care, deliver Medication Assisted Treatment, and meet all of the site certification and staff licensing requirements to do this work and do it well."
We are pleased to introduce the highlights of this plan here and will continue to share enhancements and updates as we move forward in this work.
“Ultimately, we need to provide dedicated programming that combines mental health and substance use services directly to our clients in our programs. We believe that by doing that, we can better close the gap and help our clients holistically move forward in recovery – and dramatically improve their lives.”
Overarching Goals
Our vision for our SUTS plan is ambitious. We want to:
Increase quality of care
Increase access to care
Increase strategies for effective care
Reduce the stigma of care
Nurture a safe space for change
Create many options and avenues for clients to make positive behavioral change
Enable staff and clients to work proactively and collaboratively toward recovery
SUTS Plan at a Glance
What's New in SUTS
Director of SUTS: Scott Madover
/To help us better address co-occurring conditions company-wide, we appointed Scott Madover, Ph.D., to take on the role of Telecare’s Director for Specialty Product Services, Substance Use Treatment Services (SUTS).
"We knew we really needed to focus on substance use, and ensure that we were capable and doing our very best to meet those needs. We thought the best way to do that was to hire a dedicated leader, and that's Scott Madover," said Faith Richie, SVP of Development at Telecare.
In addition to working with the Development and Operations departments at Telecare to create plans for how co-occurring programming could better serve our clients, Scott will also assist with Telecare’s planning efforts so that our services are aligned with parity requirements and SUTS funding in multiple states. He will also ensure that Co-Occurring Education Groups (COEG) curriculum is available at all our product types, and recommend new standards for our existing programs so that they are co-occurring capable.
Scott’s clinical training and program leadership experience coupled with his wealth of knowledge in co-occurring disorders positions him very well for this role.
Before accepting his role as the new SUTS Director, Scott has helped lead many of Telecare’s integrated care efforts, including the development and roll out of COEG, our first company-wide substance use education program, and the design and implementation of Telecare’s first pay for success program. He also helped design and oversee the CHANGES program, our first program specifically designed to support people with co-occurring mental illness/substance use needs. Scott has also served as Regional Director of Operations in the Bay Area.
Telecare is a Best Place to Work!
/






Telecare has been named a Best Place to Work (BPTW) in the Bay Area by the San Francisco Business Times. Staff from STRIDES/STEPS/STAGES, Villa Fairmont, Redwood Place, Sausal Creek, Cordilleras, Willow Rock, Gladman Mental Health Rehabilitation Center, Heritage Psychiatric Health Center, Morton Bakar Center, and CHANGES attended the celebration in San Francisco on Tuesday, April 18.
Out of 537 applicants, only the top 130 companies were chosen for this award based on BPTW employee engagement survey responses. This is the 15th time we have been recognized on this list.
This year, we ranked ninth in the Largest Employer category. We would like to say thank you to all our staff for making Telecare a great place to work! We are truly honored.
Links we Love: Mental Health Month
/May is Mental Health Month. Show that you are #IntoMentalHealth and check out the following for awareness events taking place next month:
Health & Wellness Curriculum | A Whole Person Care Status Report
/Telecare has a long-range plan for expanding and deepening its Whole Person Care (WPC) efforts. We began by examining
co-occurring conditions—educating providers and ensuring that Telecare’s Co-Occurring Education Group is available in all our programs. Right now, we are laying the foundation for future efforts by focusing on health literacy.
We recognize that behavioral health providers need support as they work with clients to address their physical and substance use issues. In May 2016, Telecare introduced Phase 2 of our Whole Person Care initiative: health literacy. The Health & Wellness Curriculum consists of eight online modules on topics such as Diabetes, Cholesterol, Blood Pressure, Managing Our Stress Response, Tobacco Use, and more. Each module is accompanied by visually engaging and easy-to-follow handouts that staff can use to engage clients in conversation about these health concerns.
Though we’re still early in our company-wide implementation, the feedback so far is promising. Here is an update on our progress, as of April 2017. Below, you’ll find:
Where We’re Going: Implementation Timeline & Status Update
What We’re Seeing: Early Discoveries From the Field
More Info: Whole Person Care Goals
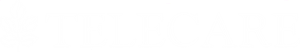
Implementation Timeline & Status Update
Right now, we are working on Phase 2: health literacy. Telecare’s programs have the flexibility to implement the health and wellness literacy curriculum at their own pace, but all programs must complete the curriculum by April 2018. Here is a snapshot of our progress over the last year.
Early Discoveries from the Field
We spoke to staff at three Telecare programs that are moving quickly to fully implement the Health & Wellness Curriculum, a 16-hour, online training program that provides staff with basic knowledge about the chronic health conditions that our clients most commonly face. Here’s what staff have told us about the curriculum’s impact so far.
We're Increasing Linkages to Primary Care
Erich Stevens, Registered Nurse
San Diego Gateway to Recovery
Early discoveries:
More conversations happening
More linkage to primary care
More physical health therapy
How the curriculum has helped:
"I think the modules and quick reference tools for use in the field have been extremely helpful to case managers and other non-nursing staff in better understanding these health issues and how to assist clients with them, which has typically been up to the nursing staff alone."
Why do it:
“It gives us more ways to help clients reach a higher level of wellness.”
Clients Are Taking More Initiative in Setting Doctor Appointments
Tienna Jackson, Team Lead
Gateway to Recovery
Early discoveries:
Clients willing to make primary care appointments
More physical health therapy
Increase in health conversations
How the curriculum has helped:
“The worksheets that were available with each module were given to members to help support them in whatever their hopes and dreams are in regards to their health and wellness.”
Why do it:
"It reinforces to our staff the importance of addressing both the medical and mental health aspects of recovery with our members, and really, it has been working. Our clinicians and nurses are coming back with stories of how they tell people the importance of seeing a doctor, and members are open to making appointments with their primary care provider on the spot."
We’re About to Help Clients Better Understand How Physical Health & Mental Health are Connected
Rocio Perez, Clinician, Los Angeles Older Adults
Early discoveries:
Handouts help show clients how mental and physical health are connected
Increased efforts towards self-care
How the curriculum has helped:
“The Health & Wellness Curriculum has been especially helpful partnered with psychoeducation. One example is around diabetes. Many of our members are diabetic, and they don’t know what it is to be diabetic, or how it affects your mental health. Having the handouts have made it easier to talk with clients about the different ways to address living and dealing with physical ailments.”
Why do it:
“For me, being mentally OK and being physically OK go together, which is how we have implemented it in our office, and I see it working.”
Whole Person Care: Big Picture
NatCon 2017 Conference
/This month, Telecare and other health and mental health organizations from around the country came together for NatCon17 in Seattle, WA. It was Telecare's third year hosting a booth at the conference, which is sponsored by the National Council for Behavioral Health.
“Telecare was honored to support the behavioral health community at the recent NATCON Conference,” said Robert Klar, Talent Acquisition Director at Telecare. “Telecare representatives from Operations, Development, Quality and HR were proud to speak with industry leaders about our mission, our products, and of course to encourage them to think about joining our organization.”
Thank you to everyone who stopped by the Telecare booth!




Links We Love: March
/- "When you are emotionally connected to your peers in recovery, you stand the best chance of being protected from the compulsion to use and do things that get you into trouble with your illness." Patrick Kennedy and Glenn Close discuss mental health and advocacy work with the New York Times.
- Mental Health America (MHA) has partnered with Booster.com, a free crowdfunding platform, to launch its first campaign to inspire individuals to "Fight in the Open."
New Leadership Announcements: March
/New Hires
Promotions
FROST: A Targeted Risk Assessment for Criminogenic Needs
/In April 2017, Telecare will begin training and preparation to use the FROST assessment in all criminal justice-based programs to help identify people at high risk of recidivism.
“We’re testing the FROST because we need to know which criminogenic needs are highest for our members, so that we are able to drive the appropriate interventions and treatment,” said Gary Hubbard, Vice President of Operations of Southern California and Arizona.
“Studies have shown that programs that target high criminogenic needs with members have a higher success rate and reduced recidivism.”
What Is FROST?
The assessment is called the Field Re-Assessment of the Offender Screening Tool (FROST).
Why the FROST Assessment?
Telecare’s Justice Involved Mental Health (JIMH) subcommittee chose the FROST because:
It is quick to complete
It can be administered by non-licensed staff
It measures for criminogenic risks
It is reasonable in cost
According to Hubbard, the subcommittee chose the FROST over another potential tool used by the Arizona court system— the Offender Screening Tool (OST) — because the OST was a pre-release measure. The FROST, by contrast, is used in the community and measures the eight criminogenic need areas that can lead to recidivism.
FROST SCORING
Frost Training
Telecare’s clinical leadership team will attend a free FROST training provided by the Arizona Supreme Court staff on April 11. Telecare's leadership will also participate in a train-the-trainer event that will be offered in the fall to build the expertise to distribute the FROST more widely to our existing JIMH programs.
Expanding Our Assisted Outpatient Treatment Services in Orange County
/Orange County AOT Facility in downtown Santa Ana
On March 7, Telecare’s Orange County Assisted Outpatient Treatment (AOT) program in Santa Ana, CA, moved into its new facility to accommodate their recent service capacity increase from 25 to 120 persons.
"Our amazing team will continue to offer services in the community, but we are so excited to have this new program site for members to feel included, safe, and valued," said Anna Bowes, Administrator for the Orange County AOT program. "The team is really looking forward to creating a community with our members. We plan to start an art gallery and offer gardening on our patio."
Originally co-located with Orange County STEPS, the Orange County AOT program is now located directly across from the Central Justice Center in downtown Santa Ana.
The space will serve as an important resource for providing more personalized care. "Now that we are closer to the Central Justice Center, we can offer hearings with an AOT judge at the program for our members who are not as comfortable at the courthouse,” Anna said. “We are also currently working with Orange County Health Care Agency and Genoa Healthcare to have an on-site pharmacy. We hope this service will increase access and efficiency in getting members connected with their medications.”
For many members in the program, access to the proper care and resources can mean a world of difference. "I have been with other programs in the county and have left the state because I had a difficult time with the program rules," said an AOT graduate. "I felt like I as being pushed around a lot and I had a hard time living."
"Ever since I’ve been with AOT, I began making a comeback," he said. "I like AOT program a lot— it has been easy and the staff are very nice. I haven’t been to the hospital in almost five months and I received psychiatry and medication services with the help of AOT."
The member's mother is especially thankful for the services her son has received. "I feel like I have my son back," she said. Although the member graduated, he has chosen to remain in the program voluntarily.
The Orange County AOT program launched in October 2014. It was Telecare’s first Laura’s Law program and has seen eight clients graduate since it opened—one of which has been connected with outside Full Service Partnership (FSP) programs or psychiatrists for continued support in their recovery, while the other seven remain with the program on a voluntary basis.
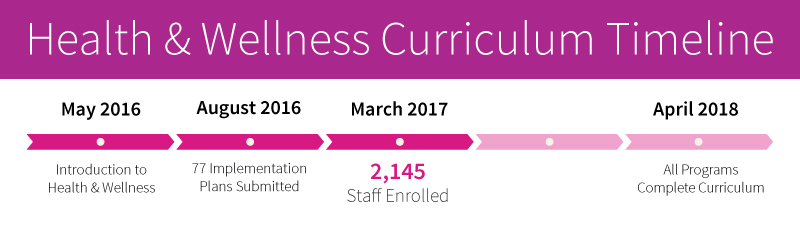
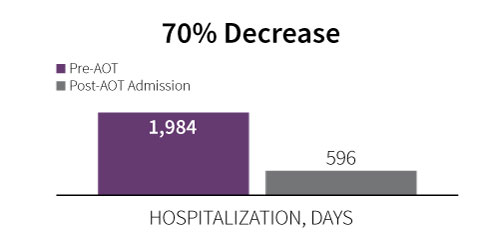
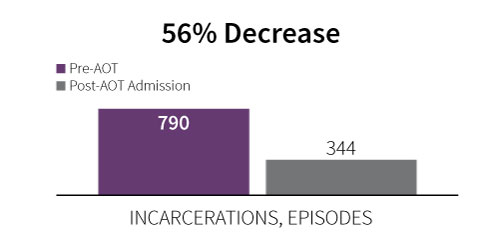
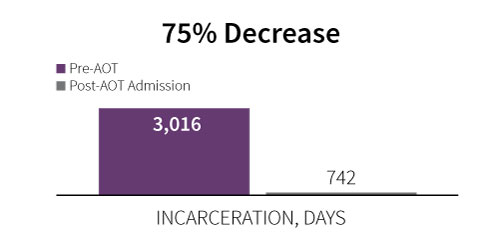
2017 Data
The information below compares hospitalization and incarceration statistics of members before and after they have been admitted to the OC AOT program from July 2016 to February 2017.
Learn More:
For more information on our JIMH programs, click here.
Read more about the early success of the OC AOT program from our Court-Ordered Newsletter.