NatCon 2018 Presentation: Pay for Success
/In 2017, Telecare opened the nation's first mental health Pay for Success (PFS) program in Santa Clara County, California, called Partners in Wellness.
At NatCon2018, Telecare hosted a lunch and learn presentation sharing initial results from our PFS program, an overview of the PFS model, a clinical overview of the program, and learnings for other systems interested in possible implementation. We are pleased to share the presentation and findings below.
Alternative Payment Models:
Pay for Success
Initial Results
In the first year of operation, Partners in Wellness saved more than $508,482 above the target savings. The program reduced usage well over the target rate for all services, including 81% over the target of psychiatric emergency services visits and 100% over the target for state hospital days. Significant clinical results were also shown: after a year, people with higher depression, psychosis, and drug and alcohol use scores showed significant improvement over time. Anxiety levels (measured through screenings) also improved, as well as physical health measurements such as HDL-C scores.
PFS Model Overview
Telecare's Partners in Wellness program is an innovative six-year, performance-based contract to deliver publicly-funded services. Telecare is at risk to deliver the savings targets outlined in the contract by reducing clients' use of psychiatric hospitals, psychiatric emergency services, state hospitals, and other mental health services while also ensuring each client’s whole-person wellness. The performance targets are set to fully pay for the program (in savings) and return additional savings at the end of the six years. Dr. Keith Humphreys of Stanford University objectively evaluates the program results. From the RFP process beginning in December 2014 through the January 2017 official launch of the program, more than two years of work went into the development of this program.
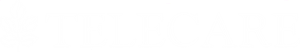
What's Different About Pay for Success?
Pay for Success programs, including Partners in Wellness, include several areas of additional measures and tools, and a higher degree of data analytics, than other programs typically provide. (Click on the chart to the right to see an outline of some of these differences.)
PFS Clinical Model Overview
The clinical care model for Partners in Wellness uses several tools to engage with consumers, also known as partners, on multiple fronts. Physical and mental health are measured through screenings and assessments, and a "whole health" care plan is created in partnership with the persons served. From there, the multidisciplinary team — including several peer specialists — works with the partner to ensure they have adequate housing, medications, physical health supports, care coordination, and assistance in developing recovery tools as they work toward their wellness and recovery goals. Data from health measures and a daily "Wellness Snapshot" are entered and used to produce a Huddle Report that prioritizes the team's treatment and intervention planning in their morning huddle. A monthly report tracks partners' progress over time. Treatments are adjusted as needs change.
Lessons Learned
One of the most important lessons we have learned in our first year of operations is how crucial it is to have a firm understanding of the community in which we are working, as well as strong relationships within that community. Factors such as other community resources, housing costs, and Conservator or Public Guardian Policies can all make a big difference in the outcomes of Pay for Success programs like Partners in Wellness.
More Information
Faith Richie, Telecare SVP of Development
Shannon Mong, Telecare Director of Innovation Initiatives
Gail Lapidus, CEO of Family and Children's Services
Download a PDF of our presentation on Pay for Success.
Partners in Wellness in San Jose, CA
Family and Children’s Services’ Women In Recovery, in Tulsa, OK
Read Mental Health Weekly's coverage of the first Pay for Success initiative to focus on mental health.